When 34-year-old Priya visited her gynecologist, complaining of debilitating periods that forced her to miss work three days every month, she wasn’t expecting to hear about a 7 cm mass in her uterus. “But I thought only older women got tumours,” she said, her voice shaking. Her doctor’s response changed everything: “These aren’t tumours in the way you’re thinking. They’re fibroids.”
If you’re reading this after a similar diagnosis, or because your symptoms have finally pushed you to seek answers, understanding the science behind uterine fibroids will help you make informed decisions about your body. Let’s dig deeper than surface-level explanations.
Uterine Fibroids: What’s Actually Happening
Uterine fibroids, medically termed leiomyomas, are monoclonal tumours arising from the smooth muscle cells of your myometrium (the muscular layer of your uterus). Here’s what makes them unique: each fibroid originates from a single aberrant myometrial cell that begins dividing uncontrollably, but in a benign pattern.
The critical distinction? Unlike malignant tumours, fibroids have well-defined borders, grow slowly, and don’t invade surrounding tissues. The malignant counterpart, leiomyosarcoma, is exceptionally rare, occurring in roughly 1 in 800-1000 women with presumed fibroids. This low risk is why most gynecologists confidently reassure patients about the benign nature of these growths.
The Four Strategic Locations
Where a fibroid grows determines everything—your symptoms, fertility impact, and treatment approach:
Intramural fibroids (70% of cases) embed within the uterine wall itself. As they enlarge, they distort the uterine cavity and increase the surface area of your endometrium (uterine lining). This is why women with intramural fibroids often experience menorrhagia, the medical term for menstrual blood loss exceeding 80ml per cycle, though most women describe it as “soaking through super pads hourly.”
Subserosal fibroids (15-20% of cases) project outward from the uterine surface into your pelvic cavity. These are the culprits behind bulk symptoms, pressure on your bladder causing urinary frequency, or compression of your rectum leading to constipation. Ironically, these fibroids may be quite large before causing heavy bleeding because they do not directly affect the endometrial cavity.
Submucosal fibroids (5-10% of cases) are the most problematic despite being less common. Protruding into the uterine cavity, even small submucosal fibroids (2-3 cm) can cause severe menorrhagia and present serious fertility challenges. They interfere with embryo implantation and are associated with recurrent miscarriages because they create an unstable environment for pregnancy.
Pedunculated fibroids grow on stalks (pedicles) extending either into the uterine cavity or outward into the pelvis. The danger here is torsion; if the stalk twists, it can cut off the blood supply, causing acute pain that often sends women to emergency departments, suspecting appendicitis or ovarian torsion.
Decoding Uterine Fibroid Size: Clinical Implications
Gynecologists don’t just measure fibroids to satisfy curiosity. Size correlates directly with treatment complexity and outcomes:


Small fibroids (less than 3 cm): Generally asymptomatic unless submucosal. These can be monitored with annual ultrasounds. Many remain stable for years.
Medium fibroids (3-8 cm): This is where symptoms typically begin. A 5 cm intramural fibroid might cause manageable heavy periods, while a 5 cm submucosal fibroid could cause hemorrhage requiring blood transfusions.
Large fibroids (8-12 cm): Classified as “bulky uterus” on ultrasound reports. At this size, even subserosal fibroids cause symptoms due to mass effect. Your uterus might measure the size of a 12-16 week pregnancy.
Giant fibroids (over 12 cm): Technically, any fibroid exceeding 10 cm is considered giant. The largest documented fibroid weighed over 60 kg, though most giant fibroids range from 1-5 kg. These require careful surgical planning and often necessitate open surgery rather than minimally invasive approaches.
What Causes Uterine Fibroids to Grow?
The honest answer to “what causes fibroids” is: we’re still piecing together a complex puzzle. But here’s what current research reveals:
Hormonal Orchestration
Estrogen and progesterone aren’t simply “female hormones”; they’re growth factors for fibroid tissue. Studies show fibroid cells have higher concentrations of estrogen and progesterone receptors compared to normal myometrium.
During pregnancy, when progesterone levels increase 10-fold, many women experience rapid fibroid growth. Conversely, after menopause, when ovarian hormone production ceases, fibroids typically shrink by 35-50% within a year. This hormonal dependency explains why GnRH agonists (medications that temporarily induce menopause) can shrink fibroids before surgery.
Genetic Predisposition
The MED12 gene mutation appears in about 70% of fibroids, while alterations in the HMGA2 gene are found in 15-20%. If your mother had fibroids, your risk increases threefold. If your sister has them, your risk is 2.5 times higher.
Lifestyle and Environmental Factors
Several modifiable risk factors influence fibroid development:
Vitamin D deficiency: Studies show women with vitamin D levels below 20 ng/mL have 2.4 times higher fibroid risk. In India, where 70-80% of the population is vitamin D deficient despite abundant sunlight (due to melanin-rich skin, clothing coverage, and indoor lifestyles), this becomes clinically relevant.
Dietary patterns: High consumption of red meat increases risk, while diets rich in cruciferous vegetables (cabbage, broccoli, cauliflower) show protective effects. These vegetables contain compounds that help metabolize estrogen more efficiently.
Obesity: Each 10 kg weight gain increases fibroid risk by 20% because adipose tissue produces estrogen through aromatase enzyme activity. This creates a self-perpetuating cycle: more fat produces more estrogen, which promotes fibroid growth.
Recognizing Uterine Fibroid Symptoms
Abnormal Uterine Bleeding: Understanding the Mechanism
Heavy menstrual bleeding (menorrhagia) isn’t just “bad periods”. Fibroids increase endometrial surface area, meaning more tissue sheds during menstruation. They also interfere with normal uterine contractions that compress blood vessels post-menstrually. The result? Prolonged, heavy bleeding can cause iron-deficiency anemia.
Clinical anemia symptoms include: fatigue that doesn’t improve with rest, shortness of breath with minimal exertion (like climbing one flight of stairs), palpitations, dizziness, and pale conjunctiva and nail beds. Many Indian women attribute these symptoms to “working too hard” or “not eating properly,” delaying diagnosis for months or years.
Bulk Symptoms: The Pressure Effect
As fibroids enlarge, they occupy space in your pelvis meant for bladder, bowel, and other structures:
- Urinary frequency: A 6 cm anterior fibroid pressing on your bladder reduces its capacity. You might urinate 10-15 times daily and wake 3-4 times nightly (nocturia).
- Urinary retention: Large fibroids can kink ureters (tubes from kidneys to bladder), causing hydronephrosis (kidney swelling), a serious complication that requires urgent intervention.
- Constipation: Posterior fibroids pressing on the rectum make bowel movements difficult, unrelated to dietary fiber intake.
- Venous compression: Very large fibroids can compress pelvic veins, causing leg swelling or deep vein thrombosis in rare cases.
Pain Patterns: What Different Types Mean
- Chronic, dull pelvic pressure: Indicates steady, gradual growth
- Acute, severe pain: Suggests red degeneration (fibroid outgrows its blood supply) or torsion of a pedunculated fibroid—both require immediate medical attention
- Dysmenorrhea (period cramps): Submucosal fibroids particularly cause severe cramping as the uterus contracts trying to expel the fibroid like a foreign body
- Dyspareunia (painful intercourse): Occurs when fibroids are located near the cervix or when the enlarged uterus is positioned abnormally
Reproductive Impact: The Fertility Dimension
Fibroids affect fertility through multiple mechanisms:
- Mechanical distortion: Submucosal fibroids distort the uterine cavity, preventing proper embryo implantation
- Altered uterine contractility: Normal peristaltic waves that help transport sperm are disrupted
- Inflammatory environment: Fibroids create local inflammation that’s hostile to embryo development
- Tubal obstruction: Large fibroids near the cornua (where the fallopian tubes meet the uterus) can block sperm or embryo passage
Uterine Fibroids Treatment: Evidence-Based Approaches
When Hormones Work
Drugs like leuprolide and goserelin create temporary medical menopause by suppressing ovarian function. Fibroids shrink 35-60% within 3-6 months. However, the catch: symptoms return and fibroids regrow once you stop the medication. These are primarily used to shrink large fibroids before surgery, making the procedure less complex and reducing blood loss.
Side effects mimic menopause: hot flashes, vaginal dryness, and bone density loss (concerning beyond 6 months of use). Adding back small amounts of estrogen-progesterone (add-back therapy) can minimize side effects while maintaining fibroid shrinkage.
Surgical Solutions
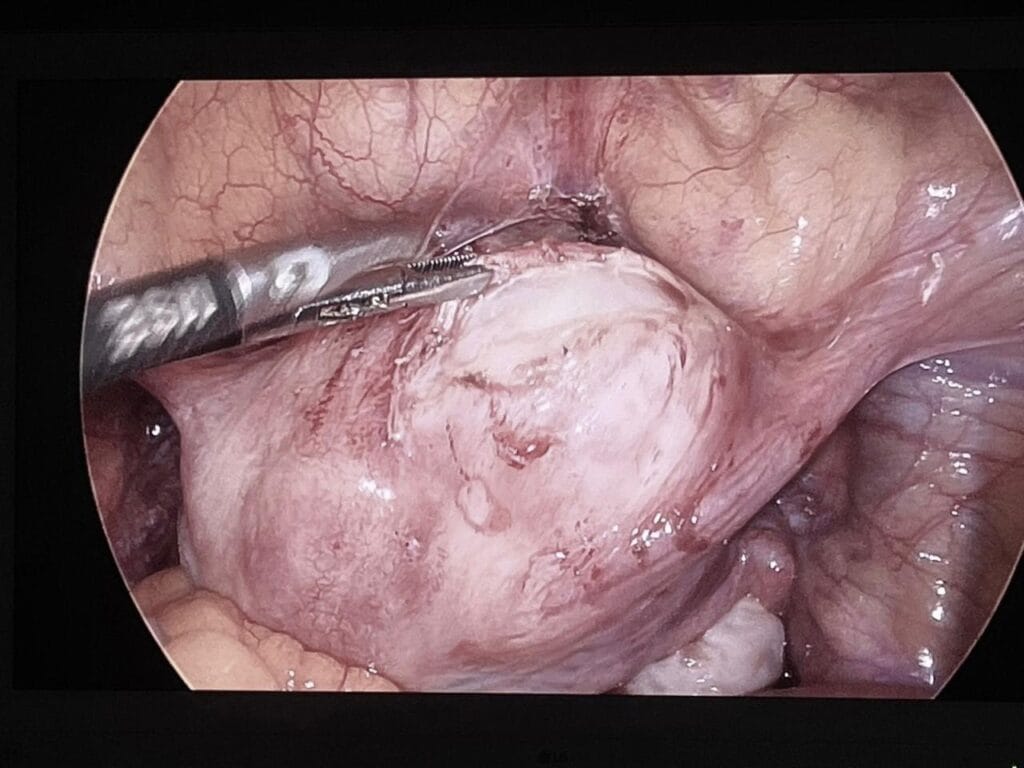
Myomectomy (Uterine Fibroid Removal Surgery)
This is the gold standard for women wanting to preserve fertility. The surgeon removes fibroids while reconstructing the uterus:
Hysteroscopic myomectomy: A hysteroscope (thin camera) is inserted through your vagina and cervix into the uterus. The fibroid is resected using electric current or a laser. No abdominal incisions, typically a day-case procedure, return to work in 3-5 days.
Laparoscopic myomectomy: For subserosal and some intramural fibroids. Using 3-4 small incisions (5-10 mm), fibroids are removed and the uterus is repaired with sutures. Requires advanced surgical skill, especially for suturing. Recovery takes 2-3 weeks.
Abdominal myomectomy (laparotomy): Required for multiple fibroids, large fibroids (over 10 cm), or complex cases. A horizontal or vertical incision gives direct access. A surgeon can remove numerous fibroids and meticulously repair the uterus. Recovery takes 4-6 weeks.
Hysterectomy: The Permanent Solution
Removal of the uterus guarantees you’ll never develop fibroids again. Modern approaches include:
Total laparoscopic hysterectomy (TLH): Removes uterus and cervix through small incisions. Faster recovery than open surgery, less post-operative pain, shorter hospital stay (1-2 days vs. 3-5 days).
Vaginal hysterectomy: Uterus removed through the vagina—no abdominal incisions, quickest recovery. Only suitable for a moderately enlarged uterus (up to 12-week pregnancy size).
Abdominal hysterectomy: Reserved for very large fibroids or when other conditions (endometriosis, adhesions) complicate surgery.
How to decide on uterine fibroid treatments?
Ask yourself and your doctor:
About your fibroids:
- How many do I have, exactly where are they located, and how large?
- Are they causing anemia? (Check your hemoglobin—normal is 12-16 g/dL for women)
- Are they affecting fertility or pregnancy outcomes?
- How fast are they growing? (Compare current and previous ultrasound reports)
About your life goals:
- Do I want biological children in the future?
- Can I manage 2-6 weeks of recovery time?
- What’s my risk tolerance for recurrence?
- How do symptoms actually impact my daily life?
About treatment options:
- What’s the success rate for my specific type and size of fibroid?
- What are the realistic risks and complications?
- If I wait 6-12 months, what’s likely to happen?
- What’s the cost, and what does my insurance cover?
Different gynecologists have different expertise and philosophical approaches. A surgeon might recommend myomectomy, while an interventional radiologist suggests UAE for the same clinical scenario.
Many women prioritize family needs over their health, delay treatment due to surgery stigma, or fear that a hysterectomy will affect their identity or marital relationship. Let’s be clear: your health isn’t negotiable. Severe anemia, chronic pain, and fertility challenges significantly impact your quality of life and ability to care for others.